
By Heather Sanders
If a picture is worth 1000 words, a three-dimensional medical image can be worth a million. And considering the vast amount of data that medical imaging machines can gather, their applications and potential in healthcare are immense. Accurate 3D images can detect cancer, help deliver life-saving interventions and guide minimally-invasive surgeries. This is where SFU computing science professor Ghassan Hamarneh hopes to help.
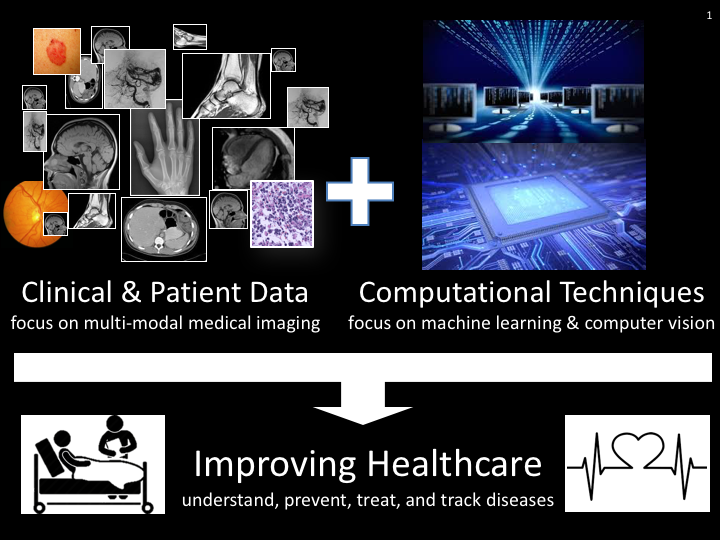
Hamarneh has been working with imaging technologies for over two decades. He leads the Medical Image Analysis Research Group, which is developing improved computer vision, machine learning and image processing methods to advance their application in healthcare and other fields. He and his team recently published Deep semantic segmentation of natural and medical images: a review, which evaluates current approaches and suggests directions for future research.
Professor Hamarneh originally studied and worked as an R&D engineer in Jordan before completing his Master’s in digital communications at Chalmers University of Technology in Sweden. It was here he developed an interest in medical imaging, and completed his doctoral studies at Chalmers and at the University of Toronto. Before joining SFU in 2003, he was a postdoctoral fellow at Toronto’s Hospital for Sick Children’s and the department of Medical Biophysics at the University of Toronto. Hamarneh keeps a busy schedule teaching, researching, running a lab and working from home with a five-year-old, but was happy to chat about his work for the Scholarly Impact of the Week.
He explained how machine learning and imaging technologies could take some of the workload off medical professionals, and the variety of reasons to do so. A physician can look at an image and make an assessment, but human judgement is subjective, and experts can differ in opinion. As mentioned, medical scanning technologies such as MRI (magnetic resonance imaging); CT (computed tomography) scan; ultrasound; positron-emission tomography (PET), etc. yield vast amounts of data. Furthermore, medical experts are expensive, and their caseloads are high.
Computer vision and data analysis adds a precision that can be quantified, says Hamarneh. A machine will give you the same result every time. Day by day, precision technology can detect minimal changes in cancerous tumours, for example, and the results are reproducible, reducing variability. While medicine is not quite ready to trust medical decisions to artificial intelligence, AI can work as a second opinion to confirm and clarify what the expert sees. “At this stage we are thinking of these technologies as alert systems, as red flags,” he says, “they support decision-making, and can point out anomalies that may have been missed.”
In Hamarneh’s recent article, semantic segmentation refers to assigning meaning to image pixels, for example, defining the precise boundaries of an object whether it’s the boundaries of a tumour, the outline of a heart muscle or border of a skin lesion. Accurate interpretations of images can inform diagnosis, guide endoscopic surgery, evaluate blood flow, and perform a host of other functions. The article provides an overview of the cutting-edge work being performed in this area, considers recent advancements and where researchers may need to focus their efforts over the next five years.
The most recent trend in computer visioning is deep learning. This is essentially training a machine to perform a task by providing diverse examples and letting it draw discoveries. For example, by providing hundreds of images along with certain algorithms, a computer can learn to recognize and diagnose cancerous lesions. “In terms of machine learning, deep learning is considered state of the art,” says Hamarneh.
Hamarneh’s lab has recently partnered with researchers from UBC to understand the role of caveolin-1 in certain types of cancers. They are using machine learning to train machines to examine super-resolution microscopic images of cell structures. They also use deep learning to determine which features stand out. “With deep learning, the machine is discovering features for you, but sometimes these features are not easily interpretable,” says Hamarneh. “We are examining interpretable AI methods, where we look at what the AI discovered and expose it for biologists to gain insight.”
As the capacity of medical computational techniques grows, so does the ability to understand, prevent, treat and track diseases. And while AI is not quite ready to take on medical decision-making, it can certainly help quantify, confirm and clarify expert opinions on those million-word images.
SFU's Scholarly Impact of the Week series does not reflect the opinions or viewpoints of the university, but those of the scholars. The timing of articles in the series is chosen weeks or months in advance, based on a published set of criteria. Any correspondence with university or world events at the time of publication is purely coincidental.
For more information, please see SFU's Code of Faculty Ethics and Responsibilities and the statement on academic freedom.