Injury surveillance in low and middle income countries (LMIC)

Injury is the biggest killer in Sub-Saharan Africa, accounting for more deaths every year than AIDS and Malaria combined. Despite this enormous human toll, injury remains under-documented and prevention efforts are under-funded. Currently few LMIC countries have the human resources to collect thorough injury data in hospitals where trauma patients are treated. Dr. Schuurman and Dr. Morad Hameed (University of British Columbia) have developed an injury surveillance registry (e.g. database) that is easy to use in low-resource hospital environments. They are working with physicians and researchers in South Africa to test the new injury registry form. In addition, they are working on prevention efforts including identification of environmental correlates related to risk of injury in LMIC.
Chronic illness and disability

Rates of chronic illness are on the rise in Canada, thereby posing a significant public health challenge. This rise is due to a number of factors, including that: Canadians are living longer but not necessarily healthier; and some diseases that were once primarily fatal can now be lived with for extended periods due to medical advances, thus rendering them chronic in nature. Dr. Crooks has an established research record in chronic illness research, and her specific focus is on understanding how people live with chronic illnesses and their potentially disabling outcomes. She presently leads a study that is examining the socio-spatial workplace environment of Canadian academics with multiple sclerosis (with Dr. Sharon Dale Stone [Lakehead University] and Dr. Michelle Owen [University of Winnipeg]), and is also involved in a study led by Dr. Kelli Stajduhar (University of Victoria) that is comparatively examining the role of empowerment in nursing practice between the chronic and palliative care contexts.
Mixed-methods analyses to determine access to palliative care
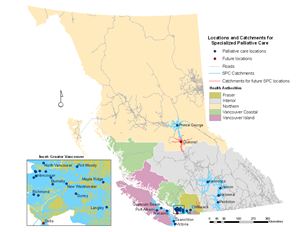
The health geography team at SFU has combined skills to develop a mixed-method approach to determining spatial access to palliative care facilities in rural British Columbia. Using a combination of road travel time, markers of isolation and vulnerability, and qualitative interviews Drs. Schuurman and Crooks are able to identify patients who are vulnerable to low/no service. They are also developing methods to determine the depth and diversity of services that patients have access to. Each of these methods assists in evaluating equity of access to health services more generally - provincially and nationally.
Drs. Schuurman and Crooks’ joint research in this area has also involved conducting interviews with formal and informal palliative care providers to better understand how access to care is experienced on-the ground. These interviews have revealed a number of important issues regarding the provision of palliative care in rural British Columbia. They have also used these qualitative interviews to refine their spatial approach to identifying communities in most need of enhancing palliative care service provision. This qualitative research has also been leading to a new focus on the provision Aboriginal-focused palliative care in particular.
Medical tourism

Medical tourism involves crossing national borders, and often continents, with the intent of pursuing medical care abroad. People often engage in this practice so that they can obtain surgeries without encountering long waiting lists or high out-of-pocket payments. Although more and more Canadians are reportedly engaging in medical tourism, little research exists on this important international health and health care issue. Dr. Crooks is presently leading a research team that is investigating the patient’s perspective in medical tourism. Her collaborators in this work are Drs. Paul Kingsbury (Simon Fraser University) and Jeremy Snyder (Simon Fraser University). The central question being asked in their research is: how do Canadians decide on medical tourism for elective surgical procedures and to what extent do their decisions reflect particular ethical considerations?
Spatial epidemiology of injury
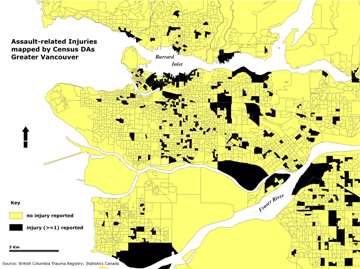
Dr. Schuurman is co-leader with Dr. Hameed of a spatial epidemiology of injury team. Over the past five years, they have developed new approaches to documenting and analyzing the distribution of injury events, social and environmental correlates with injury and access to trauma services in British Columbia. They are currently working on a national access to trauma services study as well as planning for mass casualties.
Micro-scale distribution of heat-health vulnerability air temperature and during extreme heat events
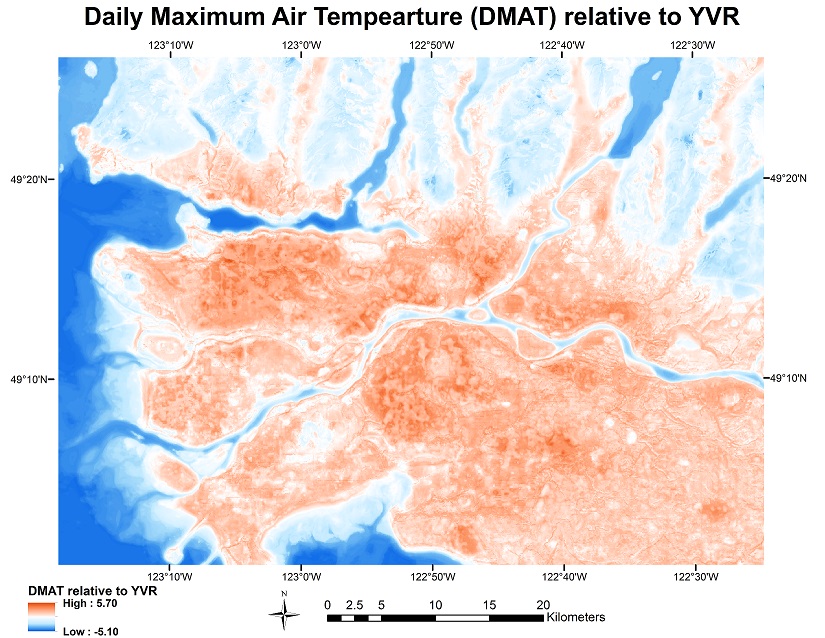
In late July and early August of 2009, a single week with extremely hot weather killed more than 100 people in the Vancouver area, more deaths than were caused by the H1N1 epidemic in all of British Columbia the same year. Such extreme heat events are expected to increase in both frequency and severity. In collaboration with Dr. Sarah Henderson (British Columbia Centre for Disease Control) this project combines spatial information on heat-health vulnerability with a new methodology developed to map micro-scale differences in air temperature across Metro Vancouver, specifically calibrated for hot summer days, to map mortality risk for a range of extreme heat scenarios. Results will assist both emergency response (e.g. by determining where to put portable water stations) as well as long-term mitigation (e.g. determine priority sites for urban greening) and adaptation (e.g. review of building codes to mandate improved insulation, air conditioning).
